A pneumothorax is a potentially dangerous lung pathology that requires rapid diagnosis and treatment. We delve into the use of lung ultrasound to detect this important condition.

SHARE
TABLE OF CONTENTS
A pneumothorax refers to the presence of air outside the lung but within the pleural cavity. This condition occurs when air builds up between the parietal and visceral pleura in the chest, exerting pressure on the lung and causing it to collapse. The extent of the collapse determines the clinical manifestation of a pneumothorax, which can vary from being asymptomatic to experiencing chest pain and shortness of breath.
In critically ill patients, lung ultrasound has shown greater accuracy as a diagnostic tool for pneumothorax compared to traditional chest X-rays, boasting a sensitivity of 88% versus 52%. With the increasing portability and user-friendly nature of ultrasound machines, lung sonography facilitates rapid evaluations of unstable patients directly at the bedside.
For assessing a pneumothorax using lung ultrasound, the patient is positioned in a semi-recumbent position with the head of the bed elevated at a 45-degree angle to promote the distribution of air toward the anterior apical region.
Use a high-frequency transducer, such as the linear probe. Place the probe in the anterior chest at the midclavicular line, right below the clavicle with the probe marker pointing toward the patient’s head.
The diagnosis of a pneumothorax involves the observation of 4 key sonographic features described below:
Lung sliding refers to the movement of the visceral pleura when it is directly adjacent to the parietal pleura. On lung ultrasound, it has been described as the appearance of “ants moving on a log” or “shimmering” of the pleural line.
In a pneumothorax, air separates the parietal and visceral pleura. Thus, you will not be able to see movement of the visceral pleura against the parietal pleura. The absence of lung sliding is very sensitive for the diagnosis of a pneumothorax. However, it is not specific as other pathologies such as pneumonia, ARDS, and bullae can all cause absent lung sliding.
Lung pulse refers to the rhythmic pleural pulsations which are observed due to the transmission of cardiac contractions to the pleura due to the apposition between the visceral and parietal pleura. In pneumothorax, as air accumulates in the pleural space and separates the lung from the chest wall, it disrupts the normal interaction between the visceral and parietal pleurae. Therefore, lung pulse may be diminished or not visualized with ultrasound.
A pneumothorax will cause an absence of vertical artifacts such as B-lines or other comet tail artifacts. These artifacts only occur when both pleural tissues (visceral and parietal) are in contact with the lung. In other words, the presence of B-lines in an area rules out a pneumothorax at that point.
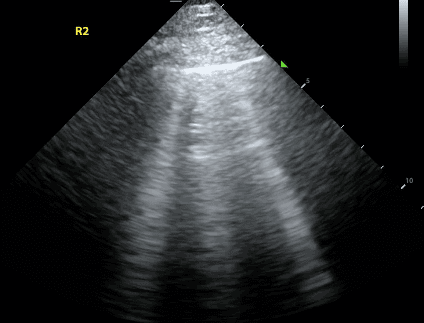
The most specific sign of a pneumothorax is the presence of a lung point. This marks the transition from normal lung sliding to absent lung sliding. Thus it marks the boundary between the collapsed and non-collapsed lung.
M-mode, or Motion mode, is a type of ultrasound modality that displays motion of a structure through time. See our post on Lung Sliding for more information on using M-mode to diagnose a pneumothorax.
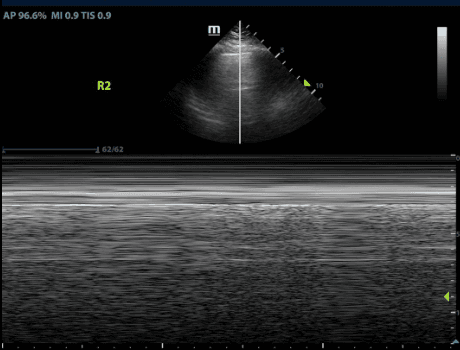
Being highly specific for pneumothorax, the lung point delineates the border of the collapsed lung and allows for determining the actual size of the condition. Remarkably specific for pneumothorax, it precisely outlines the border of the collapsed lung. Clinically, the distance is often assessed laterally between the sternum and the lung point, with larger pneumothoraces exhibiting a more lateral and posterior lung point.
Tension pneumothorax is a life-threatening type of pneumothorax. Similar to a regular pneumothorax, air enters and becomes trapped in the pleural cavity, leading to lung collapse. However, as the trapped air progressively builds up, it exerts pressure on mediastinal structures such as the heart and great vessels. This prevents blood return to the heart and can result in rapid deterioration and death.
While tension pneumothorax is largely a clinical diagnosis, certain ultrasound features can point to its presence. Notably, a fixed and dilated inferior vena cava (IVC) and the absence of respirophasic variation observed from a subcostal window suggest a pathologically elevated central venous pressure, consistent with obstructive shock. Additionally, a hyperdynamic, underfilled right heart indicates tension physiology.
In summary, a pneumothorax refers to air in the pleural cavity which causes lung collapse. Lung ultrasound outperforms traditional chest X-rays in diagnosing this possibly life-threatening condition. The 4 key features on ultrasound that allow us to diagnose a pneumothorax are: the absence of lung sliding, the absence of a lung pulse, absence of vertical artifacts, and the presence of a lung point. Use of lung ultrasound in this condition enables timely assessment and interventions, significantly impacting patient outcomes, especially in critical situations.
Husain, L. F., Hagopian, L., Wayman, D., Baker, W. E., & Carmody, K. A. (2012). Sonographic diagnosis of pneumothorax. Journal of emergencies, trauma, and shock, 5(1), 76–81. https://doi.org/10.4103/0974-2700.93116
Radiopaedia, Pneumothorax (ultrasound), accessed 22 January 2024, https://radiopaedia.org/articles/pneumothorax-ultrasound-1.
Radiopaedia, Tension pneumothorax, accessed 22 January 2024, https://radiopaedia.org/articles/tension-pneumothorax. Soni, N. J., Arntfield, R., & Kory, P. (2020). Point of care ultrasound. Elsevier.
SHARE