Point of care ultrasound is used by healthcare providers from all specialties. We dive into how it has influenced the practice and delivery of nursing care.

SHARE
TABLE OF CONTENTS
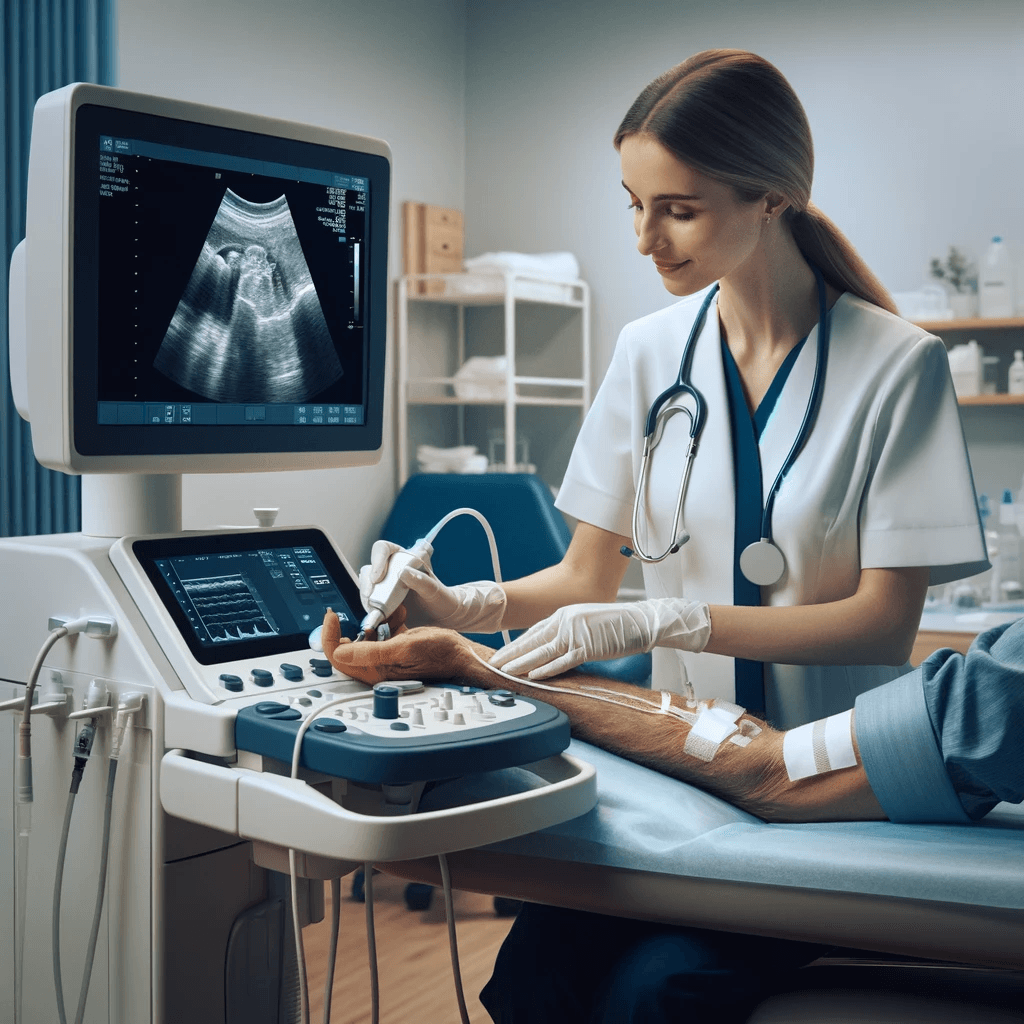
Nurses’ scope of practice has been consistently expanding in recent decades, and the integration of new technologies such as ultrasound, is no exception. Point of care ultrasound (POCUS) is safe, portable, and enhances patient care. With the increasing availability of hand-held devices, nursing-performed POCUS has become an important skill for the 21st century nurse.
Let’s explore three key areas where ultrasound improves nursing care.
The first-generation Bladder Scan BVI 2000 was released in 1986, with numerous advancements of this technology since then. Its core uses are for postvoid residual assessments, post-catheter discontinuation assessments, and prior to intermittent catheterizations. These assessments help eliminate trauma and injury associated with unnecessary catheterization or an overdistended bladder.
In 2001, a study at London Health Sciences showed that bladder scanners were highly accurate in detecting who had a distended bladder and had an important effect on the nurse’s decision on whether to proceed with catheterization. Today, bladder scanners are an integral tool used by nurses in most acute care settings.

Assessment of peripheral pulses is essential when evaluating for systemic and limb perfusion. Providers often find it challenging to detect peripheral pulses in patients with diabetes, peripheral vascular disease, sepsis, high vasopressor requirements, and those who have recently undergone cardiac procedures.
Nursing performed Doppler ultrasound technology helps quickly and accurately verify blood flow in order to rectify this problem. An investigation by Ross et al. (2007) showed that adding Doppler ultrasound to manual assessment increased accuracy of pulse assessment by 9.6% in vascular nurse specialists and 15.1% in general nurses.
Initial vascular assessment, venipuncture and insertion of peripheral IVs are core nursing skills. However, factors such as obesity, trauma, shock, and previous venous access can make it difficult to cannulate the vein. Failure to establish IV access can lead to delays in treatment and can necessitate central line placement by physicians or specialized nurses.
In recent years, nursing-led ultrasound for difficult peripheral IVs has helped mitigate these concerns, expedite patient care, and avoid escalation to specialized providers for routine procedures. A randomized controlled trial conducted by Bahl et al. demonstrated that a nurse using an ultrasound-guided technique had a 76% success rate in placing a functional IV compared to 56% success rate using the traditional palpation technique in patients with difficult vascular access.
Over the years, as ultrasound technology has advanced in healthcare, nurses have demonstrated growing confidence with its use and have furthered its application into everyday practice. The question is not a matter of ‘if’ nursing ultrasound enhances patient care, but rather ‘how’ it can be integrated into practice most effectively. As new frontiers of ultrasound emerge, nursing ultrasound to assess for causes of dyspnea, hypotension, acute kidney injury, and fluid status have all become exciting areas of future investigation.
References
Wagner, M., Schmid, M. (1997) Exploring the research base and outcome measures for portable bladder ultrasound technology. MedSurg Nursing. 6 (5)
Lee, Y., Tsay, W., Lou, M., Dai, Y. (2006) The effectiveness of implementing a bladder ultrasound programme in neurosurgical units. Journal of Advanced Nursing. 57(2), 192–200
O’Farrell, B., Vandervoort, M., Bisnaire, D., Doyle-Pettypiece, P., Koopman, W., McEwan, L. (2001) Evaluation of Portable Bladder Ultrasound: Accurracy and Effect of Nursing Practice in an Acute Care Neuroscience Unit. Journal of Neuroscience Nursing. 33 (6) 301-309
Burton, S., Donovan, J., Jones, S., Meadley, B. (2022) Can Non-Physician Providers Use Ultrasound to Aid in Establishing Peripheral IV Access in Patients Who are Difficult to Cannulate? A Scoping Review. Prehospital and disaster medicine, 37(4) 535-546
Bahl, A., Pandurangadu, A., Tucker, J., Bagan, M. (2016) A randomized controlled trial assessing the use of ultrasound for nurse-performed IV placement in difficult access ED patients. American Journal of Emergency Medicine. 1950-1954
Salleras-Duran, L., Fuentes-Pumarola, C., Bosch-Borràs, N., Punset-Font, X., Sampol-Granes, F. (2016) ULTRASOUND-GUIDED PERIPHERAL VENOUS CATHETERIZATION IN EMERGENCY SERVICES. Journal of Emergency Nursing. 42 (4) 338-343
Ross, L., Banerjee, P., Rocker, M., Townsedn, E., Williams, R., Gill, E., Winter, R., Lewis, M. (2007) Doppler ultrasound improved pulse identification. The diabetic food journal. 10(3) 148-154
Houghton, K., Greenwood, J., Robinson, T., (2018) Learning from experience and sharing knowledge: doppler training for nurses to improve pedal pulse assessment. The British Medical Ultrasound Society.
Alavi, A., Sibbald, R., Nabavizadeh, R., Valaei, F., Coutts, P., Mayer, D. (2015) Audible handheld Doppler ultrasound determines reliable and inexpensive exclusion of significant peripheral arterial disease. Vascular. 23(6) 561-672
SHARE