Lung ultrasound has the potential to revolutionize prehospital diagnosis and emergency care

SHARE
TABLE OF CONTENTS
Emergency responders play a pivotal role in delivering immediate care and stabilizing patients in critical, time-sensitive situations. In these prehospital settings, rapid and accurate diagnosis can be lifesaving.
Generally, paramedics and EMTs make decisions based on vital signs, patient history, and physical examinations. However, these methods alone may not provide the full clinical picture. Medical imaging is essential for identifying life-threatening conditions early, yet in prehospital environments, limited time and resources often prevent the use of tools like chest X-rays or CT scans. Offering lung ultrasounds in pre-hospital settings gives an additional accurate assessment tool in the prehospital diagnosis of patients with torso trauma/issues. As a result, lung ultrasound (LUS) is emerging as a fast, safe, and accessible diagnostic alternative in the field.
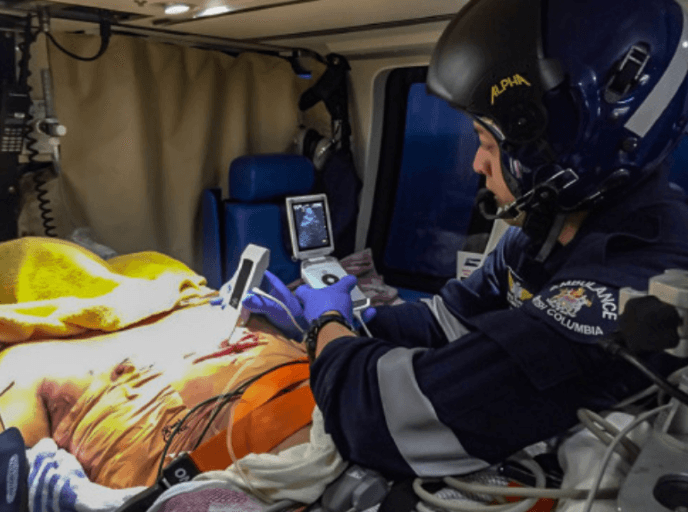
[Screenshot from SonoSite's video on ultrasound technology (SonoSite, 2011)]
Prehospital lung ultrasound offers significant diagnostic value for identifying thoracic emergencies such as pneumothorax and acute heart failure (AHF). A study by the Medical University of Lodz in Poland demonstrated that lung ultrasounds performed by paramedics for patients experiencing dyspnea aligned with hospital diagnoses in 90.91% of cases and emergency department diagnoses in 88.64%. Notably, the average exam duration was just 63.66 seconds, underlining LUS as a highly efficient and accurate tool in emergency care.
Diagnosing acute heart failure in the field presents unique challenges due to its variable and overlapping symptoms, often being misdiagnosed as pneumonia or asthma. Early recognition is critical to improve quality of life and to save treatment costs. Time constraints in prehospital care can result in delayed or insufficient treatment. A study by the Indiana University School of Medicine found that LUS achieved a prehospital diagnostic accuracy of 85% for AHF. Effectively, the use of LUS increased the rate of correct treatment from 14% to 53%, highlighting its potential to significantly improve patient outcomes.
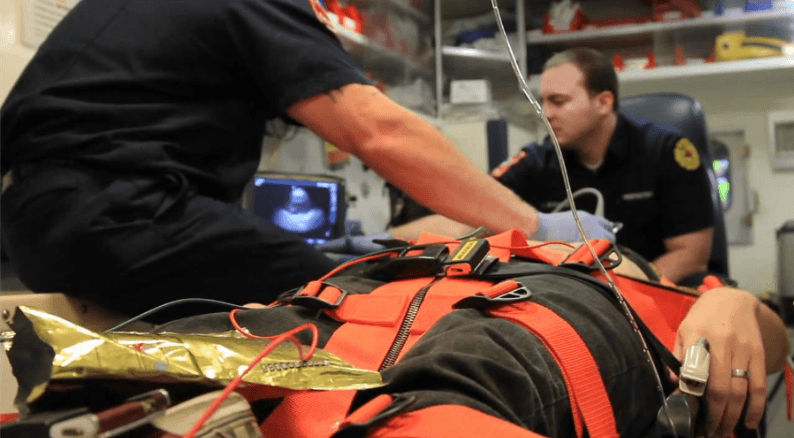
[Image reproduced from Fales et al. (2020), showing paramedic ultrasound training in practice]
Conversely, the accuracy of diagnostic ultrasound relies heavily on the operator’s skill in both execution and interpretation. But when paired with Deep Breathe’s AI-powered software, the automated deployment methods will allow for user independence and the elimination of the need for extensive training. Previously stated, the Medical University of Lodz recorded an average exam time of 63.66 seconds to diagnose a cause of dyspnea, in contrast, Deep Breathe’s technology’s diagnoses reliably in real time, allowing quicker treatment and triage.
A Deep Breathe study evaluating the accuracy of physicians identifying the lung sliding artifact in both B and M-mode was 59%. Significantly more effective is Deep Breathe’s machine learning, which was determined to range from 92-94%, an increase of 35% when determining life-threatening pneumothorax. These findings demonstrate that prehospital lung ultrasound combined with Deep Breathe’s machine learning, are revolutionizing the way in which thoracic emergencies are diagnosed, allowing for immediate, accurate, and efficient initial treatment, saving both time and resources.
Russell FM, Supples M, Tamhankar O, Liao M, Finnegan P. Prehospital lung ultrasound in acute heart failure: Impact on diagnosis and treatment. Acad Emerg Med. 2024; 31: 42-48. doi:10.1111/acem.14811
Pietersen, P.I., Mikkelsen, S., Lassen, A.T. et al. Quality of focused thoracic ultrasound performed by emergency medical technicians and paramedics in a prehospital setting: a feasibility study. Scand J Trauma Resusc Emerg Med 29, 40 (2021). https://doi.org/10.1186/s13049-021-00856-8
Kowalczyk D, Turkowiak M, Piotrowski WJ, Rosiak O, Białas AJ. Ultrasound on the Frontlines: Empowering Paramedics with Lung Ultrasound for Dyspnea Diagnosis in Adults-A Pilot Study. Diagnostics (Basel). 2023 Nov 9;13(22):3412. doi: 10.3390/diagnostics13223412. PMID: 37998549; PMCID: PMC10670426.
Russell, F. M. (2024, November 21). Study: Prehospital Lung Ultrasound Improves Diagnoses of Acute Heart Failure. JEMS. Retrieved July 8, 2025, from https://www.jems.com/patient-care/study-prehospital-lung-ultrasound-improves-diagnoses-of-acute-heart-failure/
Pertz, M. (2011, August 23). Field Medicine: EMS and Sonosite Ultrasound. YouTube. Retrieved July 8, 2025, from https://www.youtube.com/watch?v=4ylZffY5EpE
Prager R, Fiedler HC, Smith D, Wu D, Arntfield R. Interrater Agreement of Physicians Identifying Lung Sliding Artifact on B-Mode And M-Mode Point of Care Ultrasound (POCUS). POCUS J. 2025 Apr 15;10(1):92-98. doi: 10.24908/pocusj.v10i01.17807. PMID: 40342679; PMCID: PMC12057470.
Fales, W. D., Miller, J. B., Perera, P., Das, S. K., Bair, A., & Kline, J. A. (2020). A blended prehospital ultrasound curriculum for critical care paramedics. Prehospital Emergency Care, 24(2), 247–252. https://doi.org/10.1016/j.prehos.2019.10.006
SHARE